Before antibiotics were discovered, there wasn’t much in physicians’ arsenals to fight microbes. Diseases like strep throat and ear infections sometimes led to heart complications and hearing impairment; and infections related to childbirth were rampant. Antibiotics offered a new frontier in medicine.
However, when antibiotics are overprescribed or used incorrectly, it causes more problems in the long run.
“We are seeing more and more antibiotic resistance,” said Richard Martinello MD, an infectious diseases specialist with Yale New Haven Health. “When antibiotics are taken incorrectly, it can allow the bacteria to modify their structure in a way that renders a particular class of antibiotics ineffective. Eventually this can reduce our options for treating infections.”
In addition to creating smarter bacteria that are immune to the drugs that are designed to kill them, taking antibiotics when unnecessary can result in unpleasant side effects such as diarrhea, yeast infections or weakened connective tissues.
“A balance of bacteria live in our intestines. When you change the internal bacteria landscape, you can set yourself up for potentially needing more intense forms of antibiotics,” said Dr. Martinello.
When to avoid antibiotics
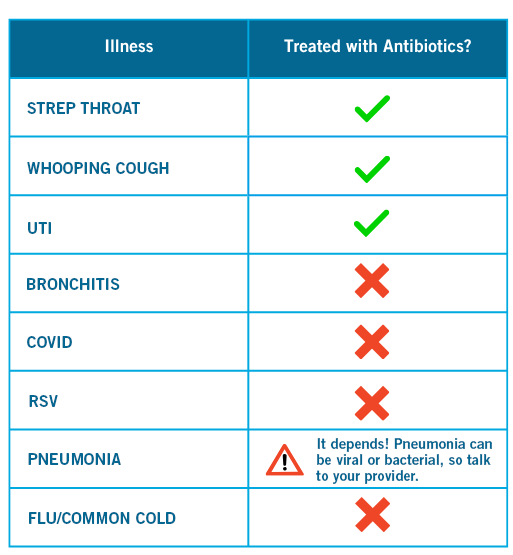
Antibiotics do not work on viruses. This means that you should not take them to treat colds, sore throats (unless you have a confirmed strep infection) or the flu.
“Studies show that antibiotics will do nothing for viral infections,” Dr. Martinello said. “One study involved researchers infecting participants with the virus that causes the common cold and giving half of them antibiotics. There was no difference in recovery between the people given antibiotics and people who took nothing. Colds can take weeks to clear up and no antibiotic can change the course of a virus.”
Dr. Martinello explains that when people take an unnecessary antibiotic for a cold or flu, they will often get better over time anyway because their immune system took care of the virus naturally. However, they incorrectly assume that the medication was the cure.
Is it bacterial or viral?
It can be a challenge for physicians to quickly assess if your infection is viral or bacterial. In many cases it isn’t easy to tell the difference without confirmation from a lab, which can take days.
“Physicians have to do an individual risk calculation every time they prescribe an antibiotic,” Dr. Martinello said. “Some cases require a culture and sometimes it is more prudent to go ahead and give the antibiotic. It takes clinical expertise to make this kind of decision.”
This is one reason why sharing antibiotics is a big mistake. No hand-off of medication can replace a doctor’s evaluation and advice.
When you need to take an antibiotic
When antibiotics are prescribed, ask if the medication should be taken with food or on an empty stomach. According to Dr. Martinello, it may be helpful to take yogurt and/or other probiotic foods with live cultures to ease stomach and intestinal issues that are sometimes related to antibiotic medications.
In addition, it’s important for those who think they may have a penicillin allergy to get confirmation from an allergist since this allergy can limit your options for certain medications.
When you start a course of antibiotics, take them exactly as prescribed. You may start to feel better before the medication is gone, and it can be tempting to stop taking it.
However, Dr. Martinello says you should continue taking all of the medication to ensure the infection is cleared and prevent it from coming back.
Disposing of medications
If you have any expired or unused medications, talk to a pharmacist about how to safely dispose of them or follow these tips.